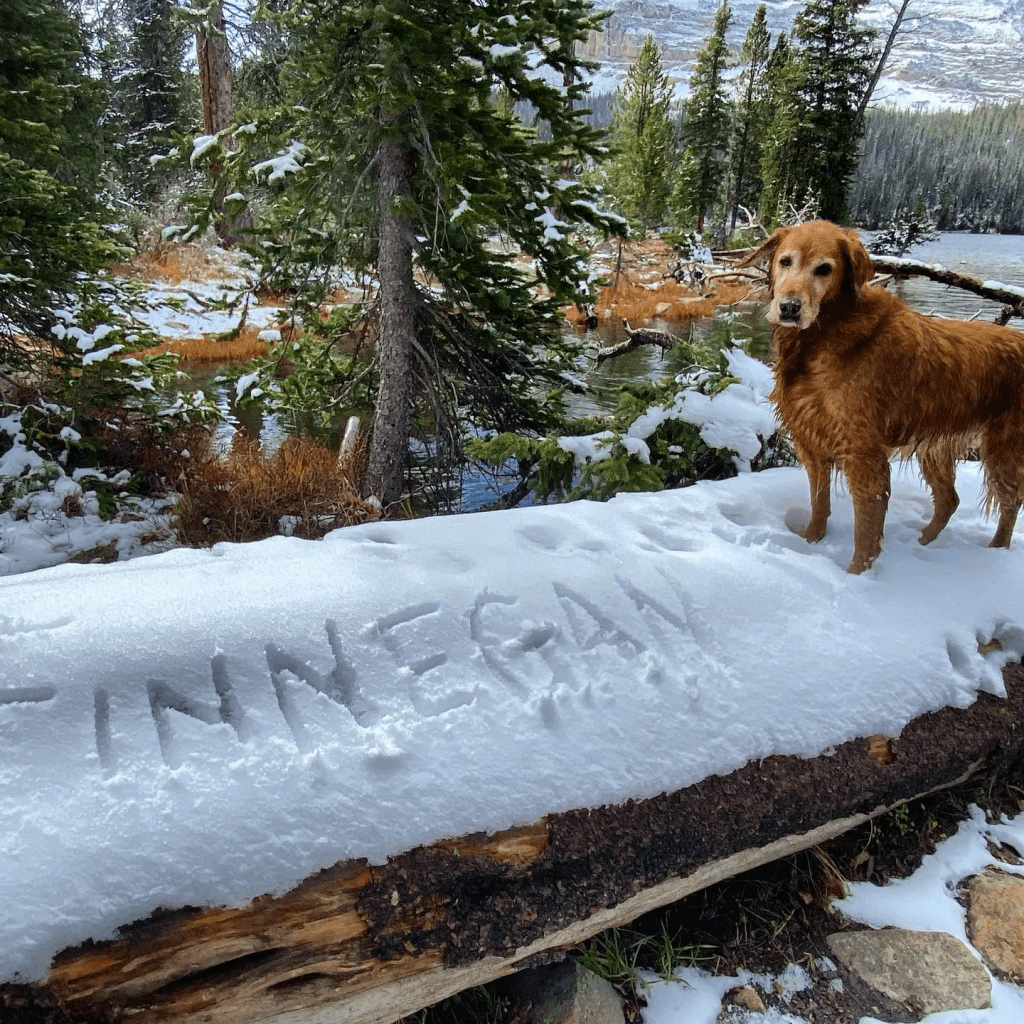
Lost in the noise of the 2025 holiday season was a story that should have attracted more attention. A New York woman, Amanda Reynolds, is taking the Internal Revenue Service (USA) to court stating that her Golden Retriever, Finnegan, is a dependent for all intents and purposes and should be a tax deduction like any human child would be.
This case goes to the heart of how households and family life are changing. The nuclear family is long gone and more adults are opting to care for pets as opposed to human children. Dogs are sentient and entirely dependent upon us – so why aren’t they considered a dependent for taxes? They require feeding and medical care – much the same as any human child.
In New Zealand, for example, under 13 year old children receive free medical care. Not so for the under 13 canines..
There will be issues of traceability if this case – facing huge hurdles – succeeds. A child is given a Social Security Number and can be tracked through school records, for example. It’s harder to track the legitimate existence of a dog and one who is properly cared for.
I look forward to seeing how this case develops…
______________
Americans love their pets. Dogs sleep at the foot of the bed, cats rule entire households, and pet photos and videos draw millions of likes on social media. It’s no surprise, then, that nearly all U.S. pet owners (97%) say their pets are part of their family.
While millions of U.S. households (about 94 million families) own one or more pets, pets are not considered part of the family for tax purposes. A recently filed case in district court aims to change that. Amanda Reynolds, an attorney licensed in New York and Utah who focuses largely on civil litigation insurance defense, recently filed a complaint in the Eastern District of New York, together with Finnegan Mary Reynolds. The catch? Finnegan is Amanda’s dog.
Amanda Reynolds
Background and Facts
Reynolds says that Finnegan, her eight-year-old golden retriever, is entirely dependent on her for food, shelter, medical care, training, transportation, and daily living. Finnegan has no independent income, resides exclusively with her, and has annual expenses exceeding $5,000. That means, Reynolds argues, that Finnegan satisfies every meaningful element of dependency recognized under section 152 of the Internal Revenue Code—except for being human. As a result, Reynolds has asked the court to determine whether pets can be recognized as non-human dependents under federal tax law.
According to the complaint, while dogs are legally classified as property, that does not fully reflect their role within families and households. Reynolds says that Finnegan’s care responsibilities mirror, and sometimes surpass, those of human dependents. Reynolds writes that “For all intents and purposes, Finnegan is like a daughter, and is definitely a ‘dependent’.”
Despite this, Reynolds notes, the tax code doesn’t allow relief for taxpayers who shoulder the financial burden of companion animals, even though it provides various credits and deductions—such as the Child Tax Credit, Dependent Care Credit, and Earned Income Tax Credit—for human dependents.
Reynolds claims this results in an arbitrary and unfair tax burden since taxpayers who provide financial support for human dependents get the benefit of tax breaks, while dog owners who provide similar levels of care receive none. This unequal treatment, she says, lacks a rational basis, especially considering the IRS’s own recognition that some animals—specifically, service dogs—may qualify for tax advantages. Reynolds argues that, from a financial standpoint, there is no real difference between service animals and companion animals.
The lawsuit alleges that the current tax law violates both the Equal Protection Clause and the Takings Clause. The Equal Protection Clause is part of the 14th Amendment of the Constitution and says that a government must apply its laws fairly and cannot treat people differently without a valid reason. The Takings Clause is part of the 5th Amendment and requires just compensation for private property.
Treating similarly situated taxpayers differently solely based on whether their dependents are human, Reynolds says, is discrimination. And, she claims that denying a tax break for the support of pets constitutes a wrongful taking because the lack of an available deduction results in a higher tax bill. Taking all of that into consideration, Reynolds says, justifies recognizing dogs as “quasi-citizens entitled to limited civil recognition, including dependency status for tax purposes.”
It may sound far-fetched, but Reynolds argues “this case is not frivolous or meritless” and warrants serious consideration by the court.
Procedural Issues
The court does not appear inclined to take up the matter. Magistrate Judge James M. Wicks granted a motion to stay discovery pending the IRS’s anticipated motion to dismiss. (Magistrate judges are appointed by the district judges of the court. In most districts, they handle pretrial motions and hearings in civil and criminal cases. While most civil cases are tried by district judges, magistrate judges may also preside over civil trials if all parties agree.)
A motion to stay discovery is a formal request to pause the discovery process in a lawsuit. Discovery happens early on in a lawsuit. As part of discovery, the parties exchange information and evidence, including document requests and depositions. It can be time-consuming and expensive, which is why a defendant may ask the court to stay discovery when a motion to dismiss is pending or anticipated (as here) and there are threshold legal issues that could end the case entirely (also as here).
The goal of a stay of discovery is to avoid unnecessary costs and effort while the court determines whether a case can or should move forward. It does not decide the case’s merits but simply pauses information gathering until the fundamental legal questions are resolved.
The Ruling So Far
Under the Federal Rule of Civil Procedure, discovery can be stayed for “good cause,” but simply filing—or planning to file—a motion to dismiss does not automatically qualify. Courts usually consider at least three factors: whether the defendant has shown that the claims are likely without merit, whether discovery would be extensive or burdensome, and whether a stay would unfairly prejudice the non-moving party.
Applying those principles here, Wicks concluded that a stay is warranted. Specifically, Wicks found that the IRS made a substantial showing that the original complaint is unlikely to survive a motion to dismiss. In a detailed pre-motion conference letter, the feds outlined several defects in the complaint, including lack of standing, improper service, and failure to state a claim as a matter of law. (Reynolds did not oppose or respond to that letter, according to court documents.)
Lack Of Standing
Standing is a legal term that refers to your right to bring a lawsuit or have a court hear your case—to be heard, you typically have to show that another party has harmed you and that the only fix for that harm can be found in court. The idea is to ensure that matters that end up in court aren’t frivolous and are raised by the right parties.
In her lawsuit, Reynolds does not allege that she actually attempted to claim her dog as a dependent or suffered an actual injury. That raises a standing problem. There are other issues with the complaint, Wick found, that impact standing, including that the Anti-Injunction Act and the Declaratory Judgment Act generally bar challenges to tax assessments and collections. Notably, the Anti-Injunction Act prevents courts from hearing suits brought “for the purpose of restraining the assessment or collection of any tax,” while the Declaratory Judgment Act bars federal courts from issuing any declaratory relief “with respect to federal taxes.”
Improper Service
The IRS also claims improper service. In a lawsuit, service (or service of process) refers to the formal delivery of legal documents, like the summons and complaint, to the defendant. The goal of proper service is to give the defendant notice that they are being sued and to allow them an opportunity to defend themselves. Lawsuits against federal agencies, like the IRS, require strict compliance with federal rules when it comes to service, which the IRS argues did not occur here.
No Constitutional Claims
Finally, complaints aren’t allowed to proceed when “the allegations in a complaint, however true, could not raise a claim of entitlement to relief.” While Wicks didn’t officially rule on the merits of the case, he did note that the Fourteenth Amendment does not apply to federal agencies and that the Fifth Amendment takings claim is unlikely to succeed (the mere payment of taxes does not constitute a compensable taking). And, he notes that the laws and tax court precedent make clear that animals cannot qualify as dependents under section 152 of the tax code.
What Are Dependents?
Under the federal tax code, dependents are persons that you can claim on your tax return. There are two kinds of dependents: a qualifying child and a qualifying relative.
A qualifying child must be related to you (typically, your child, stepchild, foster child, sibling, or descendant), live with you for more than half the year, meet age requirements (generally under 19, under 24 if a full-time student, or permanently and totally disabled at any age), and not provide more than half of their own financial support. The child also cannot file a joint tax return with someone else (except under very limited circumstances).
A qualifying relative, despite the name, need not be related by blood—they must be a person who is related to you or lives as a member of your household for the entire year. They must receive more than half of their support from you and have gross income below an annually adjusted threshold. There is no age limit, so your elderly parent could qualify. However, your spouse is never your dependent.
The statute specifically uses the term “individual” which courts and the IRS have consistently interpreted to mean human beings. As a result, pets—no matter how much they might feel like a member of your family—don’t meet the criteria.
As for those tax benefits? Reynolds is right that claiming a dependent can result in tax-favored credits and deductions. These include the Child Tax Credit (and Additional Child Tax Credit), the Credit for Other Dependents, and the Earned Income Tax Credit. Dependents may also qualify for a favorable head-of-household filing status, which offers lower tax rates and a higher standard deduction. But there isn’t any language in case law or statutes that would allow pet owners to claim those tax breaks.
(It’s worth noting that the definition of a dependent can narrow, especially as it relates to age, depending on the specific deduction or credit you’re claiming.)
The Care Of Animals Can Be Deducted In Limited Instances
While pets can’t be claimed as dependents, the tax code permits some limited deductions for animals. For instance, expenses for service animals may qualify as medical deductions, animals used in a trade or business may generate deductible expenses (such as guard dogs), and the care of foster animals may lead to a charitable deduction.
Outside of these narrow categories, however, pet-related costs for food, veterinary care, grooming, and housing are considered personal expenses, and therefore, not deductible.
Next Steps
The case has not yet been dismissed, although it appears from the recent ruling that it will be. (The Department of Justice declined to comment on the matter.)
Reynolds, however, remains optimistic. In a statement provided to Forbes, she noted, in part, “I commenced this case out of a labor-of-love as a dog owner and pup-mom to a golden retriever whom I esteem as my own daughter, having raised her by myself while my friends got married and had children. She has been in daycare while I am at work, I have paid for her medical visits, hospital visits, food, shelter and all other facets attendant to dog ownership.”
She added that she expects the litigation to be largely paper-oriented. She’s expecting the motion to dismiss shortly and says she “will address their arguments in opposition at that time.”
For now, however, don’t expect to see dogs like Finnegan listed on Form 1040.