Scientists have made significant strides in addressing a common yet concerning issue: overweight pets. This research unveils the potential of specific probiotics to combat obesity in dogs.
Leading the charge is Dr. Younghoon Kim, a distinguished professor at Seoul National University’s Department of Agricultural Biotechnology.
Understanding pet obesity
Dr. Kim’s team, with a focus on metabolic diseases in companion animals, embarked on a mission to identify probiotics that could offer a safe, long-term treatment for dog obesity.
“The initial challenge involved selecting specific metabolic diseases for examination, leading us to focus on the prevalent issue of ‘obesity in pets,’” Dr. Kim explained.
The global trend of pet obesity is alarming, with about 50% of the pet population across various age groups being affected, particularly older pets.
Many of these pets are already receiving treatments, including dietary interventions. Dr. Kim and his team set out with a clear objective: to find probiotics that could effectively reduce body fat percentage in pets.
Tackling dog obesity with probiotics
Dr. Kim’s vision goes beyond just addressing specific health issues. He advocates for a broader recognition of the therapeutic potential of probiotics across a spectrum of diseases affecting companion animals.
“By promoting this awareness, my aspiration is to catalyze increased attention, funding and collaborative efforts in the scientific community to explore the expansive landscape of probiotic applications in pet health,” Dr. Kim stated.
To pinpoint the right probiotic candidates, the research delved into the variations in intestinal microbiota between younger and older dogs.
This investigation highlighted a decline in certain beneficial bacteria, such as lactic acid bacteria, Bifidobacterium species, and Enterococcus species in older dogs.
These findings guided the researchers in selecting specific strains for their experiment.
Two probiotics helped dogs lose weight
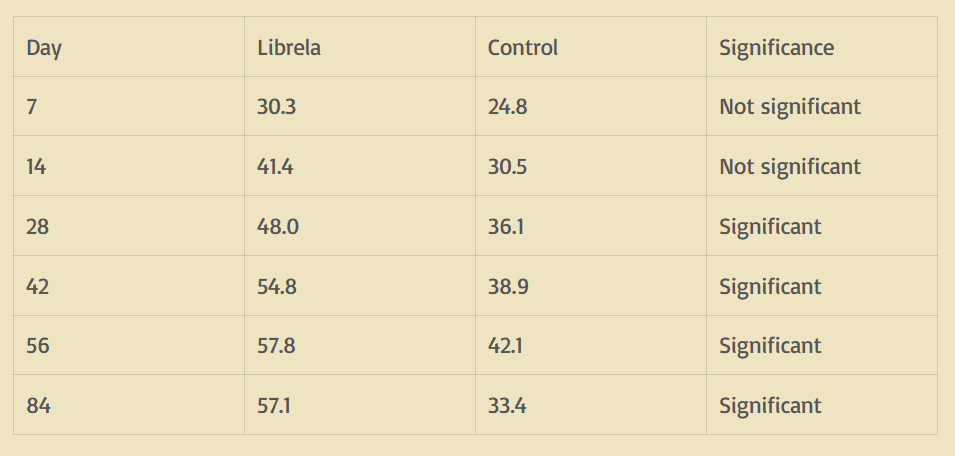
The study then progressed to its experimental phase, where two selected strains, Enterococcus faecium IDCC 2102 and Bifidobacterium lactis IDCC 4301, were administered to a group of beagles on a high-fat diet.
The results were striking. “The strains we carefully selected demonstrated remarkable success in reducing the body fat percentage in dogs,” said Kim.
These probiotics effectively reduced body weight, cut down subcutaneous fat, and boosted energy metabolism even on a high-calorie diet, shifting the body’s focus from fat storage to fat consumption.
“What set these strains apart was their ability to not only limit dietary intake or enhance excretion to reduce body weight but, more importantly, activate energy metabolism. Even when exposed to a high-calorie diet, we observed a decrease in body weight, alleviation of subcutaneous fat accumulation and an increase in energy metabolism. This confirmed a shift in the body’s metabolic orientation toward fat consumption, rather than fat accumulation,” Kim explained.
Significantly, this study also highlighted the strains’ impact on systemic inflammation and hormone metabolism.
Long-term benefits of probiotics for dogs
The dogs that received these probiotics showed reduced inflammation and improved metabolic activities, like insulin production.
The strains also increased beneficial commensal bacteria, enhancing the body’s defense mechanisms and immunity.
Dr. Kim emphasized the lasting impact of these changes, indicating sustained benefits for pets incorporating these probiotics into their health regimen. This enduring effect is pivotal in managing long-term health in pets.
With the rise in pet ownership, there’s a growing interest in health functional foods for pets, especially probiotics.
However, research in this area, particularly tailored probiotics for companion animals, lags far behind human studies.
“While types of probiotics suitable for human consumption or commercial livestock have been identified and established, the absence of standardized guidelines for companion animals is a glaring gap,” said Dr. Kim.
“Our study aimed to address this deficiency by striving to broaden the spectrum of probiotics applicable to pets across various environments.”
Promising future of pet probiotics
In summary, this important study led by Dr. Younghoon Kim marks a significant milestone in the fight against pet obesity, unveiling the remarkable potential of specific probiotics to combat this widespread issue.
By meticulously selecting and testing strains, the research team demonstrated their effectiveness in reducing body fat and enhancing metabolism in dogs, while highlighting the long-term health benefits these probiotics offer.
This research paves the way for more tailored health solutions in pet care, encouraging further exploration and development in this vital field.
It stands as a beacon of hope for pet owners worldwide, offering a new, sustainable approach to managing the health and well-being of their beloved companions.
The full study was published in the journal Microbiology Spectrum.
More about probiotics
In the realm of health and wellness, probiotics have emerged as unsung heroes, revolutionizing our understanding of gut health and beyond.
As discussed above, these live microorganisms, often referred to as “good” or “friendly” bacteria, play a critical role in maintaining a balanced intestinal microbiome, which is crucial for overall health.
Balancing the gut
Probiotics primarily work by enhancing the gut flora, which is a complex community of microorganisms living in our digestive tracts.
This boost in beneficial bacteria aids in various digestive processes and fortifies the body’s defense mechanisms against harmful pathogens.
Regular consumption of probiotics has been linked to improved digestion, enhanced immune function, and even a reduction in the risk of certain chronic diseases.
Treating digestive disorders
One of the most significant benefits of probiotics is their ability to treat and prevent gastrointestinal issues, such as irritable bowel syndrome (IBS), inflammatory bowel disease (IBD), and antibiotic-related diarrhea.
By restoring the balance of good bacteria in the gut, which can be disrupted by factors like antibiotics or poor diet, probiotics alleviate these digestive disorders.
Furthermore, emerging research suggests that probiotics may have a broader impact on our health than previously thought.
Studies indicate potential benefits in areas such as mental health, where probiotics are believed to play a role in mood regulation and reducing symptoms of depression and anxiety.
This connection, often referred to as the gut-brain axis, opens new avenues for mental health treatments.
Benefits of probiotics on humans and dogs
Probiotics also show promise in enhancing heart health by lowering LDL (bad) cholesterol levels and blood pressure.
This cardioprotective effect is another feather in the cap of these microscopic powerhouses.
Incorporating probiotics into one’s diet is relatively straightforward. They are found naturally in fermented foods such as yogurt, sauerkraut, kefir, and kimchi.
For those who prefer supplements, a wide range of probiotic capsules and powders are available on the market.
In summary, probiotics are a key component of a holistic approach to health, both for humans and dogs alike. Their wide-ranging benefits, from improving gut health to potentially boosting mental well-being, make them a valuable ally in our quest for a healthier life.
As research continues to uncover their myriad benefits, probiotics are set to play an even more prominent role in our daily health regimen.
Source: Earth.com